What are SSRIs & How do they Work? Selective Serotonin Reuptake Inhibitors Explained
Over the decades a multitude of antidepressants have been developed, and the creation of newer mechanisms of action and better safety profiles has been the driving force of pharmaceutical companies for drug development.
What are SSRIs?
Selective Serotonin Reuptake Inhibitors (“SSRIs”) are the most commonly prescribed antidepressant because of their efficacy.
But aside from efficacy, SSRIs as a family of antidepressants are “blockbusters” in large part because of their unique safety profile in the setting of overdose.
Can you Overdose on SSRIs?
Since patients with depression are prone to suicidal ideation and at risk of overdosing on antidepressant medications, earlier classes of antidepressants with a relatively high fatality rate in overdose were almost exclusively prescribed and monitored by psychiatrists.
SSRI’s changed this: there are very few recorded fatal overdoses on SSRIs, so they created and dominated the arena of primary care providers (PCPs), and not just psychiatrists, diagnosing and treating depression.
What can you Treat with SSRIs?
Offering broad therapeutic benefits, the FDA has granted approval indications for SSRIs for:
- Major Depressive Disorder (MDD)
- Premenstrual Dysphoric Disorder (PMDD)
- Bulimia Nervosa
- Generalized Anxiety Disorder (GAD) – and a broad array of other anxiety disorders
- Panic Disorder
- Post-Traumatic Stress Disorder (PTSD)
- Obsessive-Compulsive Disorder (OCD)
Not every SSRI has been granted FDA approval for the same disorders, but each SSRI can be generally used for any of the conditions other SSRIs can treat because of class equivalency.
The available FDA-approved SSRIs are:
- Prozac (fluoxetine)
- Paxil (paroxetine)
- Zoloft (sertraline)
- Luvox (fluvoxamine)
- Celexa (citalopram)
- Lexapro (escitalopram)
- Viibryd (vilazodone)
Neurons, Neurotransmitters & Electromechanical Messaging
To understand what SSRIs are and how they work, we must first understand the structure of the human brain, which components of the brain affect and regulate one’s mood, and what is the root of the chemical imbalance behind different mental health conditions.
What are Neurons? What are Neurotransmitters?
Brain cells are called “neurons.” There are 80-120 billion neurons in the human brain composed of many diverse neuron types.
Chemicals that pass information from one neuron to another are called neurotransmitters.
What do Neurons Do?
Neurons are not only chemical messengers (because of making and releasing neurotransmitters), but also electrical messengers.
There is a part of the neuron called the cell body which contains the cell’s nucleus. When this part gets stimulated by an adjacent neuron, the cell body sends an electrical excitatory current (the “message”) down its “axon” (a long, slender projection that functions like an insulated copper wire) to its “dendrite” (where neurotransmitters are stored) causing the dendrite to release the neurotransmitter (chemical messenger) downstream.
So, technically, adjacent neurons stimulate each other, sending excitatory signals to release neurotransmitters.
The Mood Circuit and Depression
The “mood circuit” is composed of serotonergic neurons (that manufacture serotonin), dopaminergic neurons (that manufacture dopamine), and noradrenergic neurons (where norepinephrine is manufactured).
The three types of mood circuit neurons arise in the upper brainstem and together form a delicate network that weaves its way through the brain and provides lateral projections, interconnections, and communication to the rest of the brain.
One of the major endpoints for the mood circuit is called the Left Dorsolateral Prefrontal Cortex.
What is The Left Dorsolateral Prefrontal Cortex?
The Left Dorsolateral Prefrontal Cortex (DLPFC) functions as a central hub and switching station to mediate brain functions in the mind and body.
The DLPFC integrates the thinking part of the brain (cortex) with other lower layers and regions throughout the brain.
Where is the DLPFC located?
The Left Dorsolateral Prefrontal Cortex is located in a relatively small area of a few square centimeters located near the top of the head. Specifically, it’s nested towards the front of the head above the temple area, and slightly to the left.
Importantly, the DLPFC is located on the outer layer of the brain, just inside the skull.
Can a Brain Scan show Brain Activity?
It is possible to do imaging studies of the brain which will show brain activity relative to how much glucose and oxygen consumption and blood flow are happening.
This in turn helps determine the overall behavior and activity of neurons – are the neurons hyperactive, normally active, or underactive?
Brain Activity in Major Depressive Disorder
In Major Depressive Disorder (MDD), proven on an average composite of imaging studies of large groups of depressed people, the neurons are dramatically underactive. As if the neurons and the entire brain have fallen asleep, there is a reduction in glucose and oxygen consumption, as well as blood flow. These brain changes contribute to what is colloquially known as the “depressed brain”.
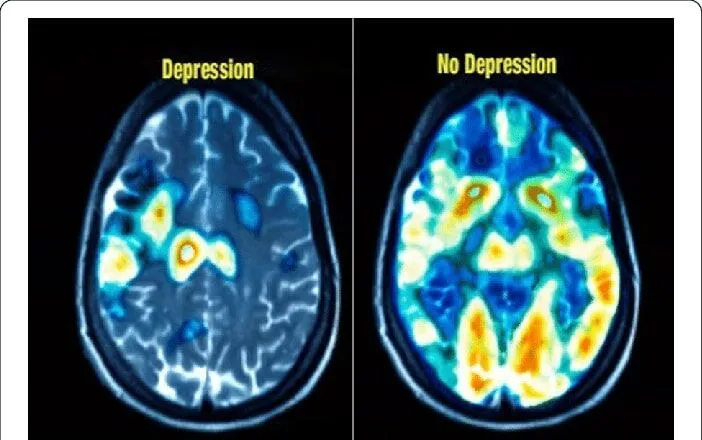
Source: Research Gate – “Classification of normal and depressed EEG signals based on centered correntropy of rhythms in empirical wavelet transform domain”
How do Depression Treatments affect Neurons and Neurotransmitters?
Treatments of depression are intended to reawaken the mood circuit of the brain. This, in turn, reawakens the entire brain. In particular, the reawakening process targets the stimulation of serotonin–, norepinephrine-, and dopamine-producing neurons in the mood circuit by raising their concentration and stimulating the effect of their specific neurotransmitter.
Any antidepressant medication essentially targets only one of the neurotransmitter types – serotonin, norepinephrine, or dopamine – usually by blocking the reuptake pump that “recycles” the neurotransmitter back into the neuron that released it.
The human body’s nervous system is well thought out and neurotransmitters are released by neurons to make a short trip downstream to the adjacent neuron, but then get recaptured by the “sending” neuron by a reuptake pump that returns the neurotransmitter back inside the neuron for later use. It is an elegant, economical system.
How do SSRIs Work?
SSRIs work by specifically blocking the serotonin reuptake pump of the serotonin neurons. This keeps higher serotonin neurotransmitter concentrations outside the neurons so there is more active serotonin messaging downstream in the nervous system.
How to Choose an SSRI
When choosing an antidepressant, it’s important to remember that there are multiple different types of antidepressants, and that SSRIs are just one option.
For patients who would likely react best to Selective Serotonin Reuptake Inhibitors, there can still be a trial-and-error phase. Two individuals with the same diagnosis can react differently to the same SSRI.
Medication Management doesn’t need to be a linear process – different SSRIs, although they have the same “task”, are absorbed and metabolized differently within the body and have a different impact and different side effects, which is why it’s important to try at least two different antidepressants before deciding that medication treatment isn’t right for you.
Your doctor will decide on the best SSRI for you based on a number of different factors, including:
- Other health conditions you have (and associated medications you may be taking)
- Your family history (whether or not a specific type of SSRI has worked for a close relative)
- Your past experience with antidepressants (if you have one)
- Possible side effects (and whether they would impact your consistency with proceeding treatment)
- Whether you’re pregnant or breastfeeding (as research on the weight of risks vs benefits of taking antidepressants while pregnant or breastfeeding is still inconclusive, so it’s approached on a case-by-case basis)
Likewise, your psychiatrist will closely monitor how well you’re responding to the medication within the first few weeks to months of taking SSRIs and decide whether to stop the medication, or perhaps try a different type of SSRI.
Below are the most commonly prescribed antidepressants at the Dr. TMS Therapy clinic.
Lexapro
My favorite SSRI to prescribe for Depression and Anxiety Disorders is Lexapro for several reasons. Lexapro is the cleanest SSRI at targeting the serotonin system with minimal effect on other unwanted targets in the body. This means greatly reduced side effects.
In addition, Lexapro is the easiest SSRI for the body to metabolize in the liver and to be eliminated by the kidneys (generally, medications are chemically broken down in the liver so they can eventually be eliminated from the body via the kidneys in the urine). Because Lexapro is liver-friendly it “plays well” (does not have many negative interactions) with other medications in the body.
Finally, Lexapro is relatively easy to start and stop in patients with minimal serotonin withdrawal.
What is Serotonin Withdrawal?
Serotonin withdrawal is possible with certain serotonin-based medications and is characterized by nausea, emotional swings, brain zaps, and dizziness when the head turns.
Celexa
Celexa is closely related to Lexapro, but it has additional side effect potential.
The reason for the increased side effect profile is that Celexa is composed of both right- and left-handed molecules. When manufacturing Celexa, the end-product medication contains both the S-isomer (left-handed molecule) and the R-isomer (right-handed molecule). The S-isomer of Citalopram is the more active therapeutic isomer, meaning it is more effective for treating depression and anxiety symptoms. Whereas, the R-isomer contained in Celexa not only has a much weaker therapeutic effect, but importantly due to its “anti-histamine” effect it is more prone to cause additional side effects such as sedation and weight gain than the S-isomer.
Lexapro, on the other hand, is further refined chemically as the less active R-isomer has been eliminated and Lexapro contains only the S-isomer (the name of Lexapro’s “escitalopram” was derived from “S-citalopram,” while Celexa contains Citalopram in its bilateral form). This makes Lexapro more effective in smaller doses, and theoretically less prone to cause effects for most individuals. Lexapro and Celexa are both available in generic form and are affordable.
Celexa is still deemed to be one of the safest antidepressants for older adults, so do not be discouraged from trying Celexa if you’ve been prescribed to take it. As any individual’s effect and side effect profile may not follow the general trends seen in the population, it is important to follow your own experience as some individuals find Celexa superior to Lexapro.
Follow your own experience with Celexa before deciding whether or not it’s right for you.
Prozac
My next favorite SSRI to prescribe is Prozac. Prozac has the advantage of being relatively more energizing for patients, ie, non-sedating, because of its pharmacological effect of enhancing the norepinephrine neurotransmitter system to a mild degree besides its stronger effect upon serotonin.
In addition, it tends to be weight-neutral and less prone to trigger SSRI weight gain (which happens slowly over time due to craving certain carbohydrates and perhaps making calories stickier).
Prozac has a long half-life (it stays in the body the longest of any SSRI before it is metabolized by the liver and eliminated by the kidneys) which means it is the least prone of all SSRIs to serotonin withdrawal upon discontinuation.
Can you get SSRIs over the counter?
SSRIs, like other antidepressants, are not over-the-counter medications – you need a prescription from a licensed physician or psychiatrist in order to take antidepressants. It’s also important to note that your psychiatrist may not deem antidepressants to be the most effective treatment plan for you.
If you are experiencing symptoms of depression and are wondering whether or not you need professional help, contact the Dr. TMS Therapy team and book a consultation at our clinic, in-person or online.

Walter G. Griffith Jr., MD, PA
Dr. Griffith earned his Undergraduate Degree from Notre Dame University and his Medical Degree from Ohio State University’s College of Medicine. He then completed his Residency in Psychiatry at Ohio’s prestigious Cleveland Clinic, and ultimately became the Chief Resident at the Cleveland Clinic in his final year of residency. After completing his residency, Dr. Griffith moved with his family to sunny Florida in 1992, where he worked at several hospitals in the early days of his career, but, ultimately, he decided to start his own outpatient Psychiatric Private Practice in Florida, where he has been working and growing the practice over the last three decades. Dr. Griffith is the Medical Director for the medical practice and oversees all of the medical clinicians who work in the practice in order to help manage the growing patient caseload at both of the medical office locations.
Request an Appointment
Our care team would love to hear from you! We want to see our patients get healthy.
This is our top priority.
- 727-577-1203
- Free Consult




