How Does Depression Affect the Brain? An Overview of the Depressed Brain
When most people think about depression, the first thoughts that typically come to mind are negative emotions and feelings of hopelessness. However, to really understand depression, it is important to realize that this condition is also associated with physical changes. Research regarding depression has led to the discovery of specific chemical messengers, known as neurotransmitters, that are involved with the development of this disorder. Imaging studies have also revealed significant structural differences between the healthy brain and the depressed brain.
Understanding the mechanism of depression and the structures that are altered by this condition helps doctors develop targeted treatment plans. This is the key to offering effective interventions that provide long-term results.
Depressed Brain: How Is It Different from a Healthy Brain?
One of the main questions that directs clinical studies about affective disorders such as depression is “how does depression affect the brain?” According to research, depression affects brain plasticity, which is described as the ability of the vast network of nerves in the brain to grow and reorganize in response to internal or external stimulation [1]. Synaptic function, which is defined as the transfer of nerve signals, is also altered due to depression.
Another major difference between a healthy brain and a depressed brain is the reduced activity of neurotransmitters and other signaling proteins in people who are experiencing depressive symptoms [2]. Neurotransmitters that regulate memory, emotion control, and stress reactions such as dopamine, serotonin, and norepinephrine are typically low in individuals who are diagnosed with depression [3]. The progression of major depression also appears to be linked to low levels of a signaling protein called brain-derived neurotrophic factor (BDNF) that regulates brain plasticity [4]. The loss of adequate neurotransmitter and signaling protein production leads to decreased brain activity.
Imaging studies, showing a depressed brain vs a normal brain have confirmed these findings by showing decreased brain activity during depressive episodes (left) and normal activity in a healthy brain (right).
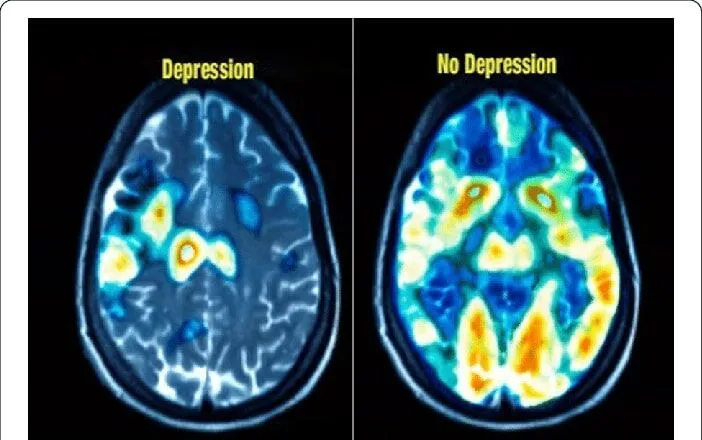
Source: Research Gate – “Classification of normal and depressed EEG signals based on centered correntropy of rhythms in empirical wavelet transform domain”
Shrinkage of Specific Brain Regions
In addition to reduced activity, research shows that the size of certain brain structures may decrease in people with depression [3]. The structures that may be affected include the following [3], [5]:
- Hippocampus – Promotes learning, memory, navigation, and spatial awareness. Hippocampal size is smaller in the depressed brain.
- Thalamus – Relays information from the outer layer of the brain, called the cerebral cortex, to the brain stem. The size and function of the thalamus are reduced in people with poorly treated depression.
- Amygdala – Regulates emotions, stress responses, and memory. The amygdala may decrease in size for some individuals with depression, while a large, hyperactive amygdala may also be observed in people with depression and anxiety [6].
- Frontal and prefrontal cortices – Frontal regions of the brain that regulate cognitive functions such as impulse control, emotional reactions, and attention. The size and activity of these structures are abnormally low in depressed people.
Fortunately, the shrinkage may be reversible, as treatments such as cognitive behavioral therapy and antidepressants help target inflammation and reduced neurotransmitter activity associated with this condition [7]. Transcranial magnetic stimulation (TMS) therapy also targets depression by exciting impaired nerve cells and brain structures with electromagnetic pulses [8]. These interventions may help reverse some of the brain changes caused by depression by reviving nerve cells and brain tissue.
Brain Inflammation
The relationship between depression and structural changes in the brain is well-established, but researchers have recently linked depression to inflammation. However, it is unclear whether depression triggers inflammatory responses or if abnormal inflammation levels contribute to the onset of depressive disorder.
Evidence suggests that inflammation levels tend to rise the longer a person is depressed [9]. This finding was demonstrated by researchers who conducted a study that involved measuring a specific protein, called translocator protein, that indicates the presence of inflammation. Researchers found that individuals who had untreated major depressive disorder (MDD) for over 10 years had significantly higher levels of translocator protein than people with untreated MDD of less than 10 years [9].
Brain inflammation can lead to brain cell death, which may cause decreased brain plasticity and tissue shrinkage. Inflammation in the brain can also disrupt neurotransmitter activity. These factors are associated with the progression of depression [3].
Overly Active Amygdala
The amygdala is one of the most common structures in the brain related to the progression of depression. This almond-shaped mass of gray matter plays a role in frontal and prefrontal cortex excitation as well as cognitive processes such as learning, emotion regulation, and memory function [1].
For people who have been diagnosed with recurrent depressive disorder or MDD, a hyperactive amygdala appears to intensify depressive symptoms [1], [3]. Hyperactivity in the amygdala also worsens intrusive thoughts, anxiety, and ruminations [3]. Researchers believe that abnormal inflammatory responses linked to depression often cause increased stress hormone (cortisol) levels that may lead to amygdala hyperactivity [10]. These findings illustrate the different depression effects on the brain.
Gray Matter Abnormalities
Depression not only affects the amygdala within the gray matter, but also leads to abnormalities in additional structures [11]. Research shows that depressed individuals who were exposed to early psychological trauma may experience a loss of gray matter in the prefrontal cortex and hippocampus [3]. This loss of gray matter appears to increase the susceptibility to depressive episodes during adulthood.
Similarly, magnetic resonance imaging (MRI) studies have demonstrated that depressed adolescents have decreased gray matter in the dorsolateral prefrontal cortex, the thalamus, and the cerebellum [11]. These are the same brain regions that are implicated in the onset and progression of MDD in adults.
Gray matter is lost as nerve cells die. Complications associated with depression, including increased inflammation and heightened cortisol levels, often lead to cell death. The dramatic neurotransmitter and structural changes that occur due to depression warrant prompt diagnosis and treatment. TMS therapy is showing promise as an effective treatment for adolescents and adults with depressive symptoms [12].
Reverse the Changes with TMS Therapy
The highly trained professionals at Dr. TMS Therapy Griffith Psychiatry use TMS technology that targets structural abnormalities, impaired nerve cells, and altered neurotransmitter activity [8], [12], [13]. TMS research shows that receiving this treatment for about five weeks helps improve symptoms of depression for many people, with response rates of about 70% and remission rates (complete recovery) of over 40% [13].
This therapeutic approach is effective for people with depression who suffer from intolerable side effects of medication, but TMS treatment can also be combined with other forms of intervention. If you’d like to learn more about how TMS therapy can help you overcome your battle with depression contact Dr. TMS Therapy Griffith Psychiatry today.

Walter G. Griffith Jr., MD, PA
Dr. Griffith earned his Undergraduate Degree from Notre Dame University and his Medical Degree from Ohio State University’s College of Medicine. He then completed his Residency in Psychiatry at Ohio’s prestigious Cleveland Clinic, and ultimately became the Chief Resident at the Cleveland Clinic in his final year of residency. After completing his residency, Dr. Griffith moved with his family to sunny Florida in 1992, where he worked at several hospitals in the early days of his career, but, ultimately, he decided to start his own outpatient Psychiatric Private Practice in Florida, where he has been working and growing the practice over the last three decades. Dr. Griffith is the Medical Director for the medical practice and oversees all of the medical clinicians who work in the practice in order to help manage the growing patient caseload at both of the medical office locations.
Request an Appointment
Our care team would love to hear from you! We want to see our patients get healthy.
This is our top priority.
- 727-577-1203
- Free Consult